Four years after COVID-19 hit the United States and sent an already strained nursing workforce reeling, staffing levels are rebounding, according to a recent study in the JAMA (Journal of the American Medical Association) Health Forum.
And the 2022 National Nursing Workforce Survey finds registered nurses are younger, more diverse, and earning a median salary of $80,000 in 2022 – up from $70,000 in 2020. It also finds an increase in education with 70% of registered nurses holding a baccalaureate degree or higher.
However, a deeper look at the lingering effects of the pandemic on the profession offers a more sobering snapshot of the nursing workforce which counts 5.2 million registered nurses with 89% working in nursing.
100,000 Nurses Left Due to the Pandemic
The National Council of State Boards of Nursing along with the National Forum of State Workforce Centers, which conducted the survey, finds that more than 200,000 experienced registered nurses left the profession between 2020 and 2022 with 100,000 of those departures directly tied to the pandemic.
Burnout, stress, and heavy workloads are cited as the major reasons for the departures. And the ripple effects remain. Twenty-eight percent of the workforce, according to the survey, plan to retire in the next five years.
This comes as the population ages, increasing the demand for health care workers overall, including nurses.
The Bureau of Labor Statistics expects the nursing field to grow 6% between 2022 and 2032, with a projected 193,100 openings for registered nurses each year over the decade. However, it’s expected that only 177,400 new nurses will be entering the workforce each year during that time, according to the U.S. Chamber of Commerce.
The majority of registered nurses work in hospitals and to get there, most need a bachelor’s degree and must pass a license exam for the state in which they work.
“Nurses are continuing to diligently do what they do every single day and that is ensure patients in our communities get the best patient care, regardless of all this other stuff that’s going on in the organization and in the profession,” says Jennifer Mensik Kennedy, Ph.D., RN, NEA-BC, FAAN, who is president of the American Nurses Association.

“We continue to have individuals go into nursing school. We continue to have nurses come into the workforce. But what we do know is that the turnover rates are continuing to be too high.”
A ‘Breaking Point’ in the Nurse Staffing Crisis
Mensik Kennedy links high turnover to poor working environments where nurses don’t feel they can provide quality care. She notes that there are a lot of opportunities for nurses – whether it be working at clinics, home health care, schools, or insurance companies. She underscores they are needed, though, in hospitals, acute care settings, and emergency departments.
“As we get further away from the heat of the moment of the pandemic, we’re forgetting about some of the things that happened that we were horribly not prepared for in organizations to support health care and support nurses,” Mensik Kennedy stresses.
She describes the staffing crisis in nursing at a ‘breaking point’ and calls for reforms, including federal legislation to set limits on the nurse-to-patient staffing ratio. There are some states that have enacted limits on how many patients a nurse can take care of at one time and there are other states proposing them.
Mensik Kennedy points out that while nursing shortages are nothing new and neither are calls for reform, there is more urgency now to create a sustainable workforce. Several organizations have formed a think tank to offer solutions. Some of the recommendations include giving nurses more voice through professional governance committees, creating healthy work environments, addressing burnout, providing more flexibility in scheduling, and rethinking models of care.
Technology Being Used to Ease Workloads
Technology is playing a part in those models. Some hospitals are using tech to cut down on nurses’ workloads.
St. Luke’s Hospital of Kansas City now has Moxi the robot helping its nursing staff by delivering supplies and medications with the goal of allowing nurses to focus more on patients.
Moxi Robots at Saint Luke’s Hospital of Kansas City
Meet Moxi, the new time-saving robot at Saint Luke’s Hospital of Kansas City. Moxi travels between departments to retrieve and deliver supplies, saving nurses lots of steps. Take an inside look at how it works.
Jefferson Health – with hospitals in and around Philadelphia – launched a Virtual Nurse Program in 2023 in an effort to support bedside nurses and reduce their workloads. The virtual nurse helps with administrative tasks such as admitting and discharging patients.
Ardent Health Services also uses virtual nurses at its affiliate Lovelace Medical Center in Albuquerque, New Mexico to assist with intakes in the emergency room.
To grow the ranks of nurses, there are incentives from both public and private entities to not only attract people to the industry but address the shortage of nursing faculty.
As part of the effort, the federal government has been committing funds to train more nurses and to provide more nursing faculty to grow the workforce.
Incentives to Attract Nurses
Efforts to create pathways, like the Nurse Corps Scholarship Program, pay for tuition and education costs for accepted applicants to earn a nursing degree in exchange for two years of service in a rural or underserved community.
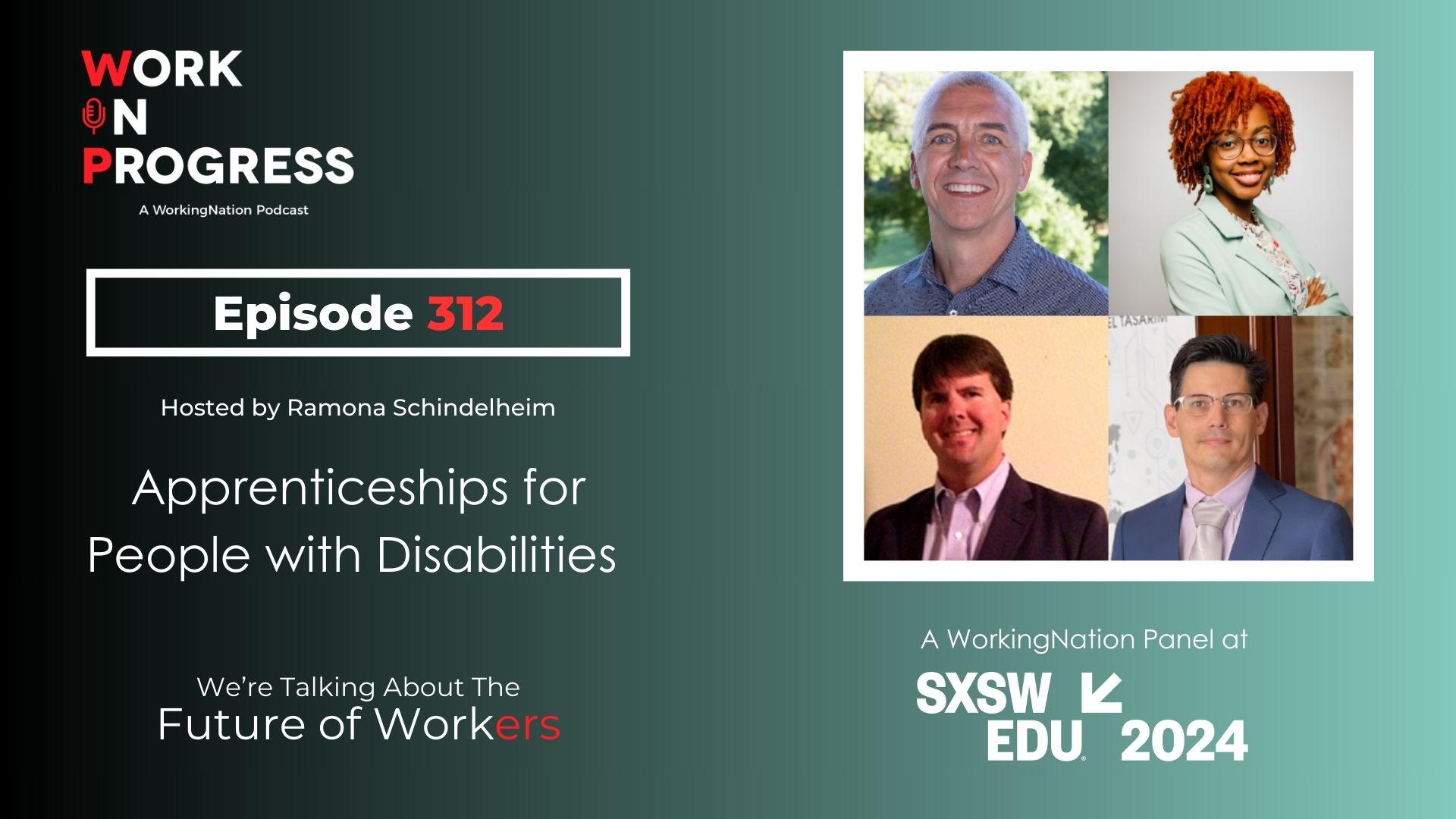
Apprenticeship programs, once linked primarily to skilled trades, are growing as a tool to attract interest in the nursing field with an earn-as you learn model. Last year, South Texas College touted a first-of-its-kind apprenticeship program in the nation – specifically geared for registered nurses.
Banner Health, which operates in six states and is headquartered in Arizona, recently announced its collaboration with Eastern Wyoming College to provide full tuition for employees and their families nationwide to earn an associate’s degree in nursing.
While it’s a sampling of some of the efforts to attract and retain nurses, ANA’s Mensik Kennedy stresses the urgency to implement sustainable solutions. She encourages people outside of the nursing field to hold health care organizations accountable for high turnover.
“We really need to get back to a point where we’re serving the community and doing what’s best for the community and putting health care first. Let’s fix the work environment for nurses and then continue to support them to come into the profession because that’s how we’re going to make this nation healthier,” says Mensik Kennedy.